12/02/2014
3D revolution at Sabancı University
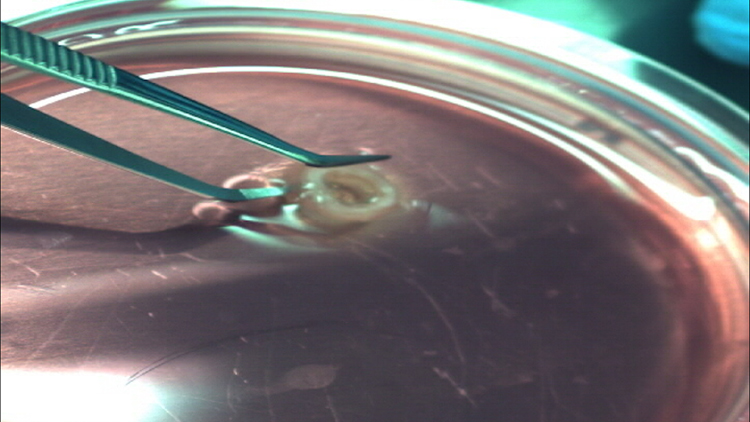
For the first time, macro-vascular tissue constructs were 3D printed by using self-supported live cells directly from medical images at the 3D Tissue and Organ Printing Lab.
Sabancı University Faculty of Engineering and Natural Sciences’ Manufacturing Systems Program professor Bahattin Koç and his team printed an artificial macro-vascular tissue construct using self-supported live cells at the 3D Tissue and Organ Printing Lab, Nanotechnology Research and Application Center (SUNUM).

The ultimate goal of the 3D tissue and organ printing group led by Prof. Bahattin Koç is to use three-dimensional bio-printers to print anatomically correct parts of or an entire tissue/organ by using the patient’s own regular cells or stem cells. Because the patient’s own cells are used, transplant rejection may not be a problem anymore.
The team was the first in Turkey and the world to use MR data to recreate an anatomically correct aortic tissue construct by using self-supporting live cell printing. The project team used live cells in a 3D bio-printer to create an anatomically correct human aortic tissue construct directly from medical images. Different from other techniques, the 3D structures printed by Sabancı University scientists are self-supported in 3D.
About the 3D Tissue and Organ Printing
The 3D Tissue and Organ Printing Group used live human dermal fibroblast cells as bio-ink to print a part of aortic tissue. Human blood vessel tissue consists of mainly three types of cells: fibroblast, endothelial and smooth muscle. Fibroblast cells are the main cell types of connective tissue. They synthesize the extracellular matrix and collagen needed for tissues. Endothelium is the thin inner layer of cells of blood vessels. Smooth muscle cells are found in inner organs such as blood vessels, esophagus and intestines. The scientists continue their efforts to 3D bio-print macro-vascular tissue constructs with fibroblasts as well as endothelial and smooth muscle cells in a bioreactor.
The interdisciplinary team of researchers and graduate students in manufacturing systems, biology, nanotechnology and materials receive support from Prof. Devrim Gözüaçık and his team from Sabancı University for cell culturing and molecular biology at the initial part of the project, Prof. Mustafa Çulha and his team from Yeditepe University for cell culturing and molecular biology, Prof. Alpay Taralp from Sabancı University for biomaterials and Prof. Bayram Koç from Gülhane Military Medical Academy in medical areas.
Sabancı University Manufacturing Systems Program Faculty Member Bahattin Koç explains the 3D Tissue and Organ Printing Project:
There are two main reasons why we focus on the aorta: First, the aorta is the largest artery in the body that caries blood to all other vessels. Since no other blood vessel is as large as the aorta, it is not possible to replace the damaged aorta by an autologous graft. Synthetic vessels made of plastic (dacron) are currently being used for treatment, but these are never as good as real human blood vessels. Moreover, if artificial tissue or organs are to be engineered, we would first need blood vessels to supply oxygen and nutrition to them. An interesting fact that few people know is that Einstein died of an aneurism in the abdominal aorta. Aneurism is the expansion of a vessel like a balloon. In later phases, this may cause the vessel to rupture, leading to internal hemorrhage and even death. As a result of our work, we may be able to produce artificial aorta using the patient’s own regular or stem cells, eliminating transplant rejection. We are at the beginnings of this work, and clinical studies may take years.
Unlike most of the previous scaffold-based tissue engineering studies, we use live cells as bio-ink in 3D printing. Using the algorithms we developed, we calculate the optimal paths to print the cells by mimicking the anatomy of the tissue to be produced. Another difference is that we print anatomically-correct tissues where all cells are self-supported in 3D. We determine how the support hydrogel structures will be used to support the cells. After determining where and how cells and their support hydrogels are printed, we save these commands to a file, and then use this file to control the bio-printer.
Our overall goal is to obtain 3D print replacement tissues and even organs that is anatomically accurate and able to meet physiological needs. We are not at the stage of building fully functional organs or tissues yet, but we are working towards this objective.
The previous research work of Bahattin Koç in 3D Tissue and Organ Printing
Sabancı University Manufacturing Systems Engineering faculty Bahattin Koç started his research on Additive Manufacturing or so-called 3D printing 16 years ago. He has been working on tissue engineering applications of 3D printing for last 7 years, starting at the University at Buffalo (SUNY). His research included the design and manufacturing of artificial skin and 3D support structures, known as scaffolds, to improve wound healing in a project supported by the US Department of Defense. Koç has been working on 3D bio-printing of artificial tissues and organs using live cells for over 2 years.
By Melek Sarı


